Hover to pan and click to magnify. Click again to pan at full screen.
Ryan Rode, MD; James Leiker, Amanda Aguila Gonzalez, MPH, Kari Harris, MD, Nicole Klaus, PhD
Ryan Rode, MD; James Leiker, Amanda Aguila Gonzalez, MPH, Kari Harris, MD, Nicole Klaus, PhD
Department of Pediatrics & Psychiatry and Behavioral Sciences Department, KU School of Medicine-Wichita
ABSTRACT
Assessment of Pediatric Mental Health Access Programs of the United States: A framework for scaling up mental healthcare access for children
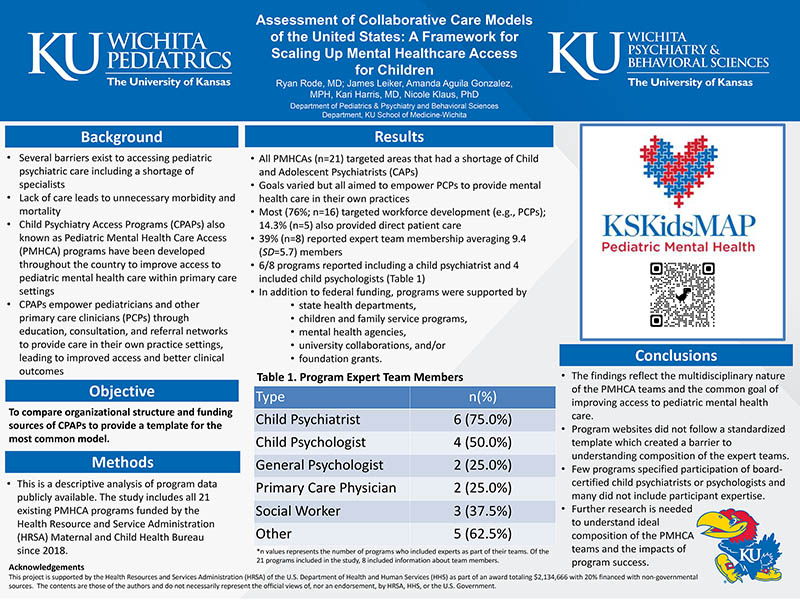
Barriers to accessing pediatric mental health care lead to unnecessary morbidity and mortality. Collaborative Care Models (CCMs) such as Pediatric Mental Health Care Access programs and Child Psychiatry Access Projects increase access to care by empowering primary care physicians and clinicians (PCPCs) to treat mental illness in their own practices. While there is well-established literature supporting CCMs, the organizational structure varies by program. Understanding characteristics of existing programs would facilitate planning and implementation efforts in other communities seeking to increase access to pediatric mental health care.
Objectives: This descriptive analysis aimed to identify characteristics of CCMs currently receiving federal funding to inform communities looking to increase access to pediatric mental health care.
Design/Methods: This is a descriptive analysis of publicly available program data regarding CCMs accessible through the HRSA Pediatric Mental Health Care Access Program Fact Sheet.
Results: A total of 21 CCMs programs were reviewed. All programs targeted areas with a shortage of Child and Adolescent Psychiatrists (CAPs). Program objectives varied, however all shared the goal of empowering PCPCs to provide mental health care within their own practices. Most (76%; n=16) targeted workforce development (e.g. PCPCs) while 14.3% (n= 5) also provided direct patient care. Only 39% (n=8) reported expert team membership. Of those who identified expert team membership, programs averaged 9.4 (SD = 5.7) members. Six of the nine programs included a child psychiatrist and four included child psychologists. In addition to federal funding, programs were supported by state health departments, children and family service programs, mental health agencies, university collaborations, and foundation grants.
Conclusion(s): CCMs demonstrated multidisciplinary team involvement and a common goal of improving access to pediatric mental health care in communities with a shortage of CAPs. All programs relied on non-HRSA funding. Program websites did not follow a standardized template which created a barrier to understanding expert team composition and exposed an opportunity for CCMs to expand available information. Few programs specified participation of board-certified child psychiatrists or psychologists and many did not include participant credentials. Further information is needed to make conclusions regarding ideal make up of CCMs.

DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE