Hover to pan and click to magnify. Click again to pan at full screen.
Natalie
Felcher RN, Jennifer Loris RN, Deanna Ochoa RN, Sarah Bernardy RN, Angela Maroon RN, Alessandra Renteria Turley RN, Debra Jones RN, Sydney Mullins RN, Kara Kidd RN, Grace Chan RN, Becky Ba st ian RN, Mihaela Blaga RN, Leonard Sterling RN
Natalie Felcher RN, Jennifer Loris RN, Deanna Ochoa RN, Sarah Bernardy RN, Angela Maroon RN, Alessandra Renteria Turley RN, Debra Jones RN, Sydney Mullins RN, Kara Kidd RN, Grace Chan RN, Becky Ba st ian RN, Mihaela Blaga RN, Leonard Sterling RN
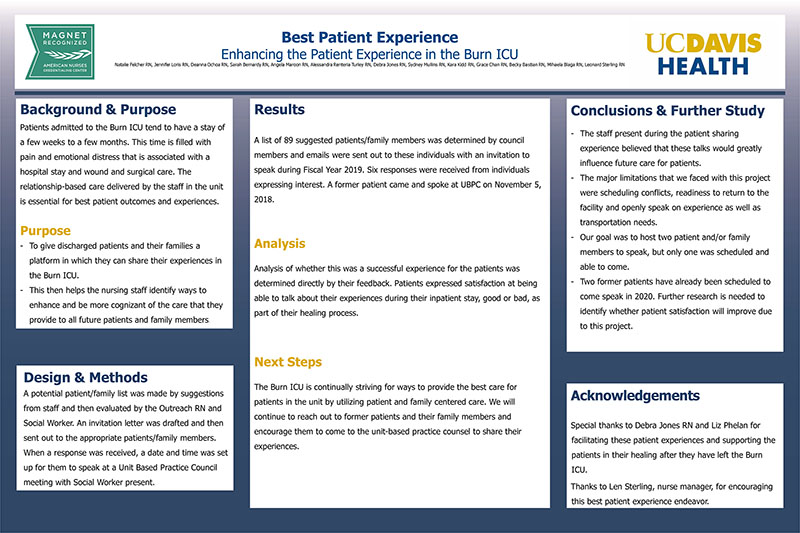
UC DAVIS HEALTH - BEST PATIENT EXPERIENCE
Background & Purpose
Patients admitted to the Burn ICU tend to have a stay of a few weeks to a few months. This time is filled with pain and emotional distress that is associated with a hospital stay and wound and surgical care. The relationship-based care delivered by the staff in the unit is essential for best patient outcomes and experiences.
Purpose
- To give discharged patients and their families a platform in which they can share their experiences in the Burn ICU.
- This then helps the nursing staff identify ways to enhance and be more cognizant of the care that they provide to all future patients and family members.
Design & Methods
A potential patient/family list was made by suggestions
from staff and then evaluated by the Outreach RN and Social Worker. An invitation letter was drafted and then sent out to the appropriate patients/family members. When a response was received, a date and time was set up for them to speak at a Unit Based Practice Council meeting with Social Worker present.
Results
A list of 89 suggested patients/family members was determined by council members and emails were sent out to these individuals with an invitation to speak during Fiscal Year 2019. Six responses were received from individuals expressing interest. A former patient came and spoke at UBPC on November 5, 2018.
Analysis
Analysis of whether this was a successful experience for the patients was determined directly by their feedback. Patients expressed satisfaction at being able to talk about their experiences during their inpatient stay, good or bad, as part of their healing process.
Next Steps
The Burn ICU is continually striving for ways to provide the best care for patients in the unit by utilizing patient and family centered care. We will continue to reach out to former patients and their family members and encourage them to come to the unit-based practice counsel to share their experiences.
Conclusions & Further Study
- The staff present during the patient sharing experience believed that these talks would greatly influence future care for patients.
- The major limitations that we faced with this project were scheduling conflicts, readiness to return to the facility and openly speak on experience as well as transportation needs.
- Our goal was to host two patient and/or family members to speak, but only one was scheduled and able to come.
- Two former patients have already been scheduled to come speak in 2020. Further research is needed to identify whether patient satisfaction will improve due to this project.
Acknowledgements
Special thanks to Debra Jones RN and Liz Phelan for facilitating these patient experiences and supporting the patients in their healing after they have left the Burn ICU.
Thanks to Len Sterling, nurse manager, for encouraging this best patient experience endeavor.

Present with Google Meet
Invite as many as 30 people, and present your poster in high definition. Transcription option is available. Free to use.
DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE