Hover to pan and click to magnify. Click again to pan at full screen.
Karen Stepp RN, MSN, PHN, RN-BC, C-OB
Karen Stepp RN, MSN, PHN, RN-BC, C-OB
UC DAVIS HEALTH - OBSTETRICS AND GYNECOLOGY
Background
Uterine atony is a major cause of postpartum hemorrhage (PPH), an emergency event that remains one of the leading causes of maternal morbidity and mortality worldwide. This study reviews a case of severe atonic PPH after a primary cesarean section resulting in an emergency peripartum hysterectomy. In the United States, prevalence studies reveal a peripartum hysterectomy rate of almost one per 1000 deliveries. Multidisciplinary collaboration utilizing effective communication is needed when responding to the severity of a stage 3 PPH.
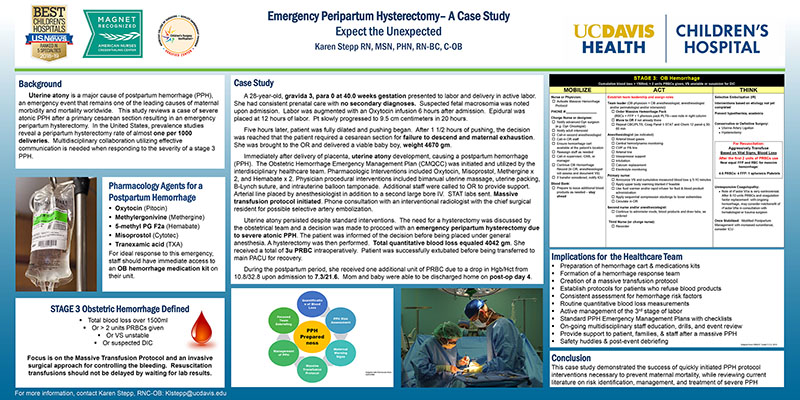
Pharmacology Agents for a Postpartum Hemorrhage
- Oxytocin (Pitocin)
- Methylergonivine (Methergine)
- 5-methyl PG F2a (Hemabate)
- Misoprostol (Cytotec)
- Tranexamic acid (TXA)
For ideal response to this emergency, staff should have immediate access to an OB hemorrhage medication kit on their unit.
STAGE 3 Obstetric Hemorrhage Defined
- Total blood loss over 1500ml
- Or > 2 units PRBCs given
- Or VS unstable
- Or suspected DIC
Focus is on the Massive Transfusion Protocol and an invasive surgical approach for controlling the bleeding. Resuscitation transfusions should not be delayed by waiting for lab results.
Case Study
A 28-year-old, gravida 3, para 0 at 40.0 weeks gestation presented to labor and delivery in active labor. She had consistent prenatal care with no secondary diagnoses. Suspected fetal macrosomia was noted upon admission. Labor was augmented with an Oxytocin infusion 6 hours after admission. Epidural was placed at 12 hours of labor. Pt slowly progressed to 9.5 cm centimeters in 20 hours.
Five hours later, patient was fully dilated and pushing began. After 1 1/2 hours of pushing, the decision was reached that the patient required a cesarean section for failure to descend and maternal exhaustion. She was brought to the OR and delivered a viable baby boy, weight 4670 gm.
Immediately after delivery of placenta, uterine atony development, causing a postpartum hemorrhage (PPH). The Obstetric Hemorrhage Emergency Management Plan (CMQCC) was initiated and utilized by the interdisciplinary healthcare team. Pharmacologic Interventions included Oxytocin, Misoprostol, Methergine x 2, and Hemabate x 2. Physician procedural interventions included bimanual uterine massage, uterine packing, B-Lynch suture, and intrauterine balloon tamponade. Additional staff were called to OR to provide support. Arterial line placed by anesthesiologist in addition to a second large bore IV. STAT labs sent. Massive transfusion protocol initiated. Phone consultation with an interventional radiologist with the chief surgical resident for possible selective artery embolization.
Uterine atony persisted despite standard interventions. The need for a hysterectomy was discussed by the obstetrical team and a decision was made to procced with an emergency peripartum hysterectomy due to severe atonic PPH. The patient was informed of the decision before being placed under general anesthesia. A hysterectomy was then performed. Total quantitative blood loss equaled 4042 gm. She received a total of 3u PRBC intraoperatively. Patient was successfully extubated before being transferred to main PACU for recovery.
During the postpartum period, she received one additional unit of PRBC due to a drop in Hgb/Hct from 10.8/32.8 upon admission to 7.3/21.6. Mom and baby were able to be discharged home on post-op day 4.
STAGE 3: OB Hemorrhage
(See poster)
Implications for the Healthcare Team
- Preparation of hemorrhage cart & medications kits
- Formation of a hemorrhage response team
- Creation of a massive transfusion protocol
- Establish protocols for patients who refuse blood products
- Consistent assessment for hemorrhage risk factors
- Routine quantitative blood loss measurements
- Active management of the 3rd stage of labor
- Standard PPH Emergency Management Plans with checklists
- On-going multidisciplinary staff education, drills, and event review
- Provide support to patient, families, & staff after a massive PPH
- Safety huddles & post-event debriefing
Conclusion
This case study demonstrated the success of quickly initiated PPH protocol interventions necessary to prevent maternal mortality, while reviewing current literature on risk identification, management, and treatment of severe PPH

Present with Google Meet
Invite as many as 30 people, and present your poster in high definition. Transcription option is available. Free to use.
DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE